The delicate balance between hunger and satiety is integral to our physical and emotional wellbeing. Difficulty controlling appetite can lead to everything from fluctuating levels of energy, mood and focus, to excessive worry, anxiety and guilt about what we’re consuming, and in more extreme cases, can also contribute to more serious health issues, like eating disorders and obesity. We’ve been taught to associate hunger with willpower, but how we experience appetite is intricately connected to the trillions of microorganisms that inhabit the lining of our digestive tract. So, how exactly does the microbiome influence our experience of hunger?
It Influences Brain Chemicals
Whilst serotonin is best known for its role as one of our ‘feel good’ hormones, it’s also a key player in appetite regulation. It turns out a whopping 90% of serotonin is produced in our gut. (1) Picture serotonin like a behind-the-scenes director, orchestrating neural circuits that regulate energy intake and expenditure while also overseeing the enjoyment of eating and happiness in general. (2) It elegantly signals when it's time to stop eating and moderates the pleasure associated with consuming food’ explains Registered Nutritionist Laura Jennings.
The health of our microbiome and the composition of our diets will influence serotonin production. From a dietary point of view, a lack of the amino acid tryptophan (serotonin's building block found mainly in protein like turkey, eggs, and salmon) can disrupt serotonin production and in turn, reduce satiety and the joy we experience from eating. It’s also important to increase our intake of polyphenols, a group of phytonutrients that have been shown to encourage the growth and health of beneficial bacteria in the gut. Think green tea, ginger and dark-coloured fruit and vegetables.
From a microbiome point of view, maintaining the balance between beneficial and pathogenic bacteria has a distinct role in appetite regulation. Our bacteria produce compounds called short-chain fatty acids (SCFAs) from the metabolism of dietary fibres, which act as chemical messengers that influence appetite regulation. (5) SCFAs like acetate and propionate stimulate the release of leptin from fat cells, one of the hormones that suppresses hunger and signals that we’re full. Consuming a diverse range of fibre rich plant foods helps boost the production of SCFA-producing bacteria in the gut, which in turn, can help with appetite control and weight management. Our microbes produce other proteins involved in hunger signalling as well, like ClpB. ClpB mimics the hormones that put the brakes on hunger by sending signals to the brain directly through our vagus nerve to tell us we’re full.(6)
It Influences Our Taste
Believe it or not, the composition of our microbiome influences our taste and cravings. A recent study indicates that individuals with lower taste sensitivity tend to overeat, while those identified as highly sensitive tasters, known as "supertasters," exhibit a greater likelihood of stopping eating when they feel full. (7) This study revealed that supertasters possess higher levels of five specific types of mouth bacteria compared to less sensitive individuals. (7) The research goes beyond the conventional understanding of food affecting the microbes in our digestive system; it suggests a reciprocal relationship where microbes influence their hosts' food choices. (8) Certain bacteria even display preferences for specific foods and fibre supplements, and when provided with their favoured foods, the abundance of these bacteria in the gut increases, implying that the food we offer our microbes can influence their cravings and specialisation. (9) For instance, consistent consumption of items like chocolate and crisps may lead to the development of microbial preferences for such foods over time. In addition to flavour, our microbial world will also influence our cravings through inflammation, insulin sensitivity and glucose control, which brings us to our next point.
It Influences Our Blood Sugar
SCFA influences appetite in another way; our blood sugar. “Butyrate-producing bacteria play a crucial role in maintaining blood sugar levels, acting as a barrier against erratic spikes and crashes,” explains Jennings. In a parallel discovery, a different strain of bacteria, Akkermansia muciniphila, essential for preventing fat accumulation and regulating sugar, was found to be lacking in individuals with prediabetes in Denmark. (11) This suggests that the gut operates as a central hub for sugar control. When our microbial community is in balance, there is harmonious control over our blood sugar levels. However, if specific key bacteria are missing, our glucose control and insulin sensitivity goes array. In addition to fibre intake and plant diversity, certain probiotic strains have been found to have antidiabetic effects by lowering fasting blood sugar, improving oxidative stress, and reducing inflammation.
The Drive Inflammation
When we think of inflammation, we usually relate it to redness, pain, and swelling, but systemic inflammation can affect us in ways we may not expect. Case in point; gut-derived inflammation can manifest as overeating. Changes to the gut's composition can cause inflammation, activating pathways involving cytokines. (14) This ongoing inflammation can disrupt signalling pathways that control appetite. (15) People with high inflammation levels might experience changes in hunger and fullness signals, potentially leading to overeating and weight gain. Moreover, a dysbiotic microbiome can cause an increase in endotoxins, which are toxic metabolites produced by bacteria that enter the bloodstream through the gut lining. This contributes to the low-grade inflammation associated with type 2 diabetes, increased stress, anxiety and fatigue; all of which in turn, can drive more hunger. (16)
How can we support our microbiome from an appetite perspective? Here are our favourite ways.
- Focus on Polyphenols: increase polyphenol-rich foods, like green tea, berries, ginger, cold pressed extra virgin olive oil, onions, red cabbage, sesame, spinach and leafy greens, turmeric, natural fermented foods
- Cut ultra-processed foods: In addition to their harmful effects on the microbiome, UPF’s have been engineered to be addictive and will alter our perception of taste.
- Work on stress reduction: chronic stress has been shown to alter the composition of the microbiome towards dysbiosis, fuelling the pathogenic bacteria that contribute to inflammation, stress and blood sugar imbalances. Whether it’s 10 minutes of mindfulness per day or breathwork before bed, it’s important to find something that works for you.
- Combat dysbiosis: increasing gut-centric foods is the first step, but for holistic microbiome support, it’s important to target the pathogenic bacteria with targeted antimicrobials. Try GI Cleanse, rich in natural antimicrobials like grapefruit seed extract, caprylic acid, cloves, black garlic extract and berberine (which is also a powerful herb for blood sugar control, found in our Metabolic Fix).
- Try a probiotic: For daily support, try Enhanced Synbiotic, which also contains cranberry and pomegranate polyphenols, which nourish Akkermansia spp as well as other beneficial bacteria. If you suffer from IBS and need advanced gut support, try Biome Restore, which boasts a therapeutic dose of Ginger and Lion’s Mane to help improve mood and reduce gut inflammation.
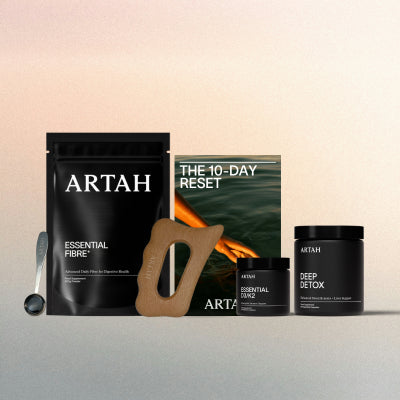
- For a complete overhaul: try The Microbiome Cleanse, a holistic nutrition programme designed to improve microbial balance and reduce symptoms associated with dysbiosis.
References
-
Barandouzi, Z.A., Lee, J., del Carmen Rosas, M. et al. Associations of neurotransmitters and the gut microbiome with emotional distress in mixed type of irritable bowel syndrome. Sci Rep 12, 1648 (2022)
-
van Galen KA, Ter Horst KW, Serlie MJ. Serotonin, food intake, and obesity. Obes Rev. 2021 Jul;22(7):e13210.
-
Pagoto SL, Spring B, McChargue D, Hitsman B, Smith M, Appelhans B, Hedeker D. Acute tryptophan depletion and sweet food consumption by overweight adults. Eat Behav. 2009 Jan;10(1):36-41
-
Han, H., Yi, B., Zhong, R. et al. From gut microbiota to host appetite: gut microbiota-derived metabolites as key regulators. Microbiome 9, 162 (2021).
-
Xiong RG, Zhou DD, Wu SX, Huang SY, Saimaiti A, Yang ZJ, Shang A, Zhao CN, Gan RY, Li HB. Health Benefits and Side Effects of Short-Chain Fatty Acids. Foods. 2022 Sep 15;11(18):2863.
-
Chambers ES, Morrison DJ, Frost G. Control of appetite and energy intake by SCFA: what are the potential underlying mechanisms? Proceedings of the Nutrition Society. 2015;74(3):328-336
-
Leung R, Covasa M. Do Gut Microbes Taste? Nutrients. 2021 Jul 27;13(8):2581.
-
Patnode ML, Beller ZW, Han MD, Cheng J, Peters SL, Terrapon N, Henrissant B, et al. Interspecies competition impacts targeted manipulation of human gut bacteria by fibre-derived glycans. Cell. 2019; 179(1); 59-73
-
Alcock J, Maley CC, Aktipis CA. Is eating behavior manipulated by the gastrointestinal microbiota? Evolutionary pressures and potential mechanisms. Bioessays. 2014 Oct;36(10):940-9.
-
Qin J, Li Y, Cai Z, Li S, Zhu J, Zhang F, Liang S, Zhang W, Guan Y, Shen D, Peng Y, Zhang D, Jie Z, Wu W, Qin Y, Xue W, Li J, Han L, Lu D, Wu P, Dai Y, Sun X, Li Z, Tang A, Zhong S, Li X, Chen W, Xu R, Wang M, Feng Q, Gong M, Yu J, Zhang Y, Zhang M, Hansen T, Sanchez G, Raes J, Falony G, Okuda S, Almeida M, LeChatelier E, Renault P, Pons N, Batto JM, Zhang Z, Chen H, Yang R, Zheng W, Li S, Yang H, Wang J, Ehrlich SD, Nielsen R, Pedersen O, Kristiansen K, Wang J. A metagenome-wide association study of gut microbiota in type 2 diabetes. Nature. 2012 Oct 4;490(7418):55-60.
-
Allin KH, Tremaroli V, Caesar R, Jensen BAH, Damgaard MTF, Bahl MI, Licht TR, Hansen TH, Nielsen T, Dantoft TM, Linneberg A, Jørgensen T, Vestergaard H, Kristiansen K, Franks PW; IMI-DIRECT consortium; Hansen T, Bäckhed F, Pedersen O. Aberrant intestinal microbiota in individuals with prediabetes. Diabetologia. 2018 Apr;61(4):810-820.
-
Utzschneider KM, Kratz M, Damman CJ, Hullar M. Mechanisms Linking the Gut Microbiome and Glucose Metabolism. J Clin Endocrinol Metab. 2016 Apr;101(4):1445-54. doi: 10.1210/jc.2015-4251. Epub 2016 Mar 3. Erratum in: J Clin Endocrinol Metab. 2016 Jun;101(6):2622
-
Cani PD, Osto M, Geurts L, Everard A. Involvement of gut microbiota in the development of low-grade inflammation and type 2 diabetes associated with obesity. Gut Microbes. 2012 Jul-Aug;3(4):279-88.
-
Al Bander Z, Nitert MD, Mousa A, Naderpoor N. The Gut Microbiota and Inflammation: An Overview. Int J Environ Res Public Health. 2020 Oct 19;17(20):7618.
-
Li Y, Jiang Q, Wang L. Appetite Regulation of TLR4-Induced Inflammatory Signaling. Front Endocrinol (Lausanne). 2021 Nov 24;12:777997.
-
Li WZ, Stirling K, Yang JJ, Zhang L. Gut microbiota and diabetes: From correlation to causality and mechanism. World J Diabetes. 2020 Jul 15;11(7):293-308.











































 SHOP ALL
SHOP ALL 






