Simrath Sehmi
13.02.2026
Bloating. That uncomfortable, puffy feeling that makes your jeans tighter, your stomach feel full, and even your mood take a hit. It’s incredibly common, yet everyone’s experience is different. Sometimes it’s that extra slice of pizza, other times it seems to appear out of nowhere. The truth is, bloating isn’t just about what you eat; factors like your gut bacteria, hormones, stress levels, and even how your body processes certain foods can all play a role. In this post, we’re breaking down five surprising reasons you might be feeling the bloat, what science says, and what you can do about it.
Dysbiosis
Dysbiosis is an imbalance in the body’s microbial communities characterised by a drop in beneficial microbes, a rise in potentially harmful ones, and/or a reduced overall diversity. In simple terms, the microbiome is off. The gastrointestinal tract is home to trillions of microbes (bacteria, fungi, viruses) that help digest food, produce nutrients, and communicate with your immune system and nervous system. We always have a mix of different types of bacteria – beneficial ones will help contribute to health, whereas harmful ones do the opposite – but in dysbiosis, the microbial community is disrupted. When this happens, we can experience bloating, gas, changes in bowel movements, and abdominal pain. (1) When “good” microbes that help break down food are reduced and other microbes proliferate, it can change how food is fermented in the gut. For example, certain bacteria produce more gas during digestion and others change how carbohydrates are broken down, which makes more gas and bloating more likely. A large meta-analysis found that people with IBS, show consistent microbiome imbalances compared to healthy individuals, including differences in major bacterial groups. (2)
What to do:
Remove irritants like UPF’s, sugar, gluten, dairy
Introduce and increase fibre from fruits, vegetables, nuts, seeds + wholegrains
Introduce daily ferments into your diet - kefir, kombucha, sauerkraut, kimchi
What to take:
G.I. Cleanse – combats the bad bacteria to bring balance to the gut
Biome Restore - live bacteria to support the growth of good bacteria.
Increased Intestinal Permeability
Our small intestine isn’t just a tube; it’s a barrier system made of multiple layers (mucus, epithelial cells, immune defences) that control what gets absorbed into the bloodstream. When this barrier functions normally it is naturally permeable, and lets nutrients in while keeping most bacteria, toxins, and partially digested food out. When this intestinal permeability increases, it becomes less selective in what it allows through into circulation. This is why it’s colloquially called ‘leaky gut.’ When this occurs, it’s common to see an increase in food intolerances, inflammation, and altered immune responses which in turn, influence digestion and sensations of fullness, gas, and bloating. There’s evidence that people with gut barrier dysfunction often overlap with symptoms seen in conditions like IBS, where bloating is a major complaint. (3)
What to do:
Remove irritants like UPF’s, sugar, gluten, dairy
Introduce and increase fibre from fruits, vegetables, nuts, seeds + wholegrains like oats.
Introduce mucilaginous foods like soaked chia seeds, flax seeds, okra,
Introduce gut lining healing foods like, aloe vera, bone broth, polyphenol rich fruits and vegetables.
What to take:
G.I. Fix - containing slippery elm and marshmallow root which are soothing and mucilaginous to support gut lining repair.
Biome Restore - live bacteria to support the growth of good bacteria.
Essential Fibre+ - fibre is essential for restoring bacterial balance in the gut and supporting a healing environment. If you aren’t able to tolerate fibre rich foods, try this before GI Fix.
Stress
Stress directly impacts our gut and can quickly lead to bloating. When the body goes into “fight or flight” mode, we releases hormones like cortisol and adrenaline. The purpose of this response is to divert energy and blood flow away from ‘non-essential’ activity so we’re ready to respond – which unfortunately includes digestion. Essentially, stress ‘switches off’ digestion; it reduces stomach acid, decreases blood flow to the intestines, and alters motility, which can leave food sitting in your gut longer than usual. This leads to more time for bacteria to ferment undigested food, producing gas and that uncomfortable bloated feeling.
Stress also affects the gut-brain axis, the two-way communication between your nervous system and gut. Chronic stress can increase gut sensitivity, making normal gas or intestinal pressure feel exaggerated. It can even alter your gut microbiome, favouring bacteria that produce more gas or contribute to inflammation, which can worsen bloating over time. (6)
What to do:
Remove irritants like UPF’s, sugar, sweetened dairy, and the more refined versions of carbohydrates
Have 3 balanced meals a day
Ensure you chew all your food well to help mechanical digestion
Practise deep breathing before and after meals to support digestion
What to take:
Digest + Debloat - to support the release of digestive enzymes
Enhanced Nootropics – to support the stress response in the body
Hormone Shifts
Many people notice that bloating worsens before or during their period, or fluctuates with other hormonal changes like menopause or thyroid imbalances. That’s not coincidence; hormones, especially oestrogen and progesterone, can directly influence digestion, fluid balance, and even how your gut microbes behave. Oestrogen isn’t just produced and discarded; our body can recycle it, and the gut plays a major role in this process. After oestrogen does its job, the liver tags it so it can be sent out of the body through the intestines. But certain gut bacteria can remove this tag, allowing oestrogen to be recycled back into circulation. Higher levels of oestrogen can slow digestion and make the body hold onto water, which can cause gas, slower gut movement, and the familiar pre-period “puffy belly.” Women with imbalanced gut bacteria, sometimes called estrobolome dysbiosis, may experience even more bloating because the recycling of oestrogen gets disrupted. Progesterone also slows gut movement, especially in the second half of the menstrual cycle, leaving food and gas in the gut longer. Since hormones and gut bacteria influence each other in a feedback loop, even small shifts can make bloating feel worse. (5)
What to do:
Remove irritants like UPF’s, sugar, sweetened dairy, and the more refined versions of carbohydrates
Introduce and increase fibre from fruits, vegetables, nuts, seeds + wholegrains
Introduce mucilaginous foods like soaked chia seeds, flax seeds, okra
What to take:
Deep Detox – to support the liver. As our hormones need to pass through the liver, we need to make sure our detoxification is efficient.
Essential Fibre+ - fibre helps bind to excess hormones and supports excretion + elimination.
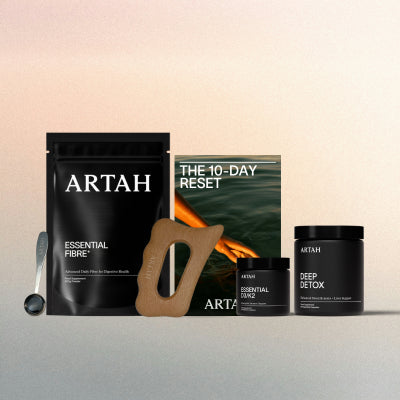
SHOP OUR GUT HEALTH SUPPLEMENTS
References
https://www.osmosis.org/answers/dysbiosis?utm_source=chatgpt.com
Wang L, Alammar N, Singh R, Nanavati J, Song Y, Chaudhary R, Mullin GE. Gut Microbial Dysbiosis in the Irritable Bowel Syndrome: A Systematic Review and Meta-Analysis of Case-Control Studies. J Acad Nutr Diet. 2020 Apr;120(4):565-586. doi: 10.1016/j.jand.2019.05.015. Epub 2019 Aug 28. PMID: 31473156.
Camilleri M. Leaky gut: mechanisms, measurement and clinical implications in humans. Gut. 2019 Aug;68(8):1516-1526. doi: 10.1136/gutjnl-2019-318427. Epub 2019 May 10. PMID: 31076401; PMCID: PMC6790068.
https://www.mayoclinic.org/diseases-conditions/small-intestinal-bacterial-overgrowth/symptoms-causes/syc-20370168?utm_source=chatgpt.com
Hu S, Ding Q, Zhang W, Kang M, Ma J, Zhao L. Gut microbial beta-glucuronidase: a vital regulator in female estrogen metabolism. Gut Microbes. 2023 Jan-Dec;15(1):2236749. doi: 10.1080/19490976.2023.2236749. PMID: 37559394; PMCID: PMC10416750.
Pritchard SE, Garsed KC, Hoad CL, Lingaya M, Banwait R, Thongborisute W, Roberts E, Costigan C, Marciani L, Gowland PA, Spiller RC. Effect of experimental stress on the small bowel and colon in healthy humans. Neurogastroenterol Motil. 2015 Apr;27(4):542-9. doi: 10.1111/nmo.12529. Epub 2015 Feb 20. PMID: 25703609; PMCID: PMC4418402.
Disclaimer: The information presented in this article is for educational purposes only and is not intended to diagnose, prevent, or treat any medical or psychological conditions. The information is not intended as medical advice, nor should it replace the advice from a doctor or qualified healthcare professional. Please do not stop, adjust, or modify your dose of any prescribed medications without the direct supervision of your healthcare practitioner.
Read More