Irritable bowel syndrome (IBS) is a complex condition that increasingly affects one in five people and is more prevalent in women.
Despite its prevalence, its causes are poorly understood and there are very few conventional treatment options, which is why it’s understandable that it’s one of the main reasons people seek out holistic and nutritional support.
First – let’s do a quick review of what it is. IBS is classified as a “syndrome” because it’s a collection of symptoms that occur together and because there are so many different ways IBS can manifest, presenting symptoms can look very different from one person to the next. There’s no specific diagnostic test to confirm you have IBS; rather, it’s diagnosed by a process of exclusion from other conditions that present with similar symptoms such as an infection, Coeliac disease, Chron’s disease, and ulcerative colitis.
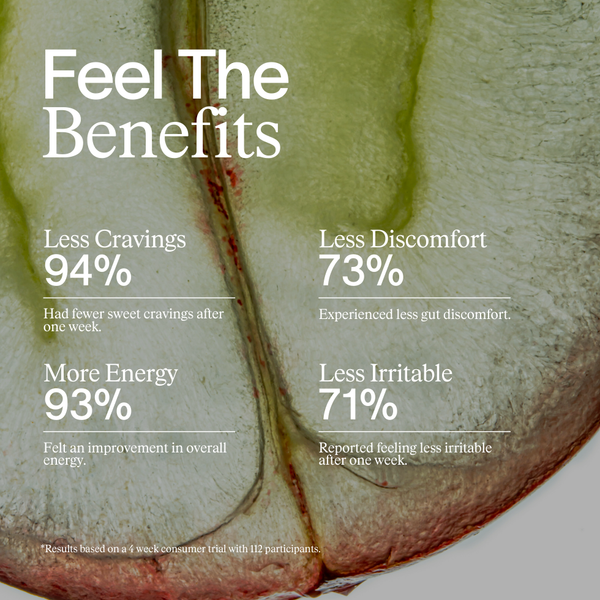
Common symptoms include bloating, abdominal cramping, urgency to pass a stool, constipation and/or diarrhoea and fatigue. Since our digestive system has a complex nervous system and a major role in mood regulation, IBS can both cause and worsen mood issues like anxiety and depression.
Depending on the type of symptoms experienced, IBS is categorised as follows:
IBS C - associated with abdominal pain, bloating and constipation
IBS D – associated with abdominal pain and urgency to pass stools and diarrhoea
IBS A – associated with the alternation between constipation and diarrhoea
IBS U - Undefined, where symptoms do not fit into the above categories
What causes IBS?
IBS rarely appears out of nowhere. Chronic antibiotic use, infection, medications, environmental factors, a stressful or emotional event, poor diet and food intolerances/ sensitivities can all cause symptoms that fall under the IBS umbrella.
Research has also linked IBS to changes to the gut microbiome known as dysbiosis, increased intestinal permeability (caused by infection, inflammation, antibiotics, or medications), as well as possible immune activation and inflammation. Dysbiosis can sometimes point towards SIBO - a condition characterized by an overgrowth of bacteria in the small intestine, so it’s important to rule this out in the diagnosis stage.
The microbiome plays a major role in digestion, motility and immunity, so once dysbiosis sets in it can be a self-perpetuating cycle that makes us more reactive to foods. Common food triggers can include FODMAPs (sugars that are poorly absorbed by the intestine), insoluble fibre (found in fruit and vegetable skins, legumes, whole grains, nuts and seeds), dairy, wheat, gluten, caffeinated and carbonated drinks, sweeteners, spicy and fatty foods.
The conventional approach for IBS is focused on symptom management, rather than addressing the root cause. It often includes laxatives for constipation, anti-motility medicines for diarrhoea, or antispasmodics to help with cramping and pain, but whilst some of these common approaches can make IBS a bit more bearable, they are a short-term fix and often come with undesirable side effects. Conversely, a holistic approach seeks to identify what is triggering your symptoms and can help provide a more comprehensive, long-term solution. Here’s where to start if you need some support.
1. First, talk to your GP
It’s important to first rule out any underlying medical condition so getting to your doctor, particularly if you’ve noticed blood in your stools, unexplained weight loss, or persistent bloating, is important. It’s also important to rule out SIBO as a cause so that you’re able to take the most appropriate nutritional approach.
2. Identify food-based triggers
Identifying food triggers of IBS can take time but is a helpful tool when it comes to symptom management. The first step is to start using a symptom tracker so that you can identify patterns to see if there is a specific food or situation that is causing a reaction. Because food intolerance or sensitivity can manifest as IBS, elimination diets can also be helpful in finding the root cause. This will involve removing specific food groups and reintroducing them one by one to look for reactions and changes in symptoms. If you’re not sure where to start, The 28-Day Reset takes you through a gluten, dairy, soy, egg, corn, and peanut-free protocol and provides guidance for what to look for whilst you introduce foods back into your regime.
Another form of an elimination diet is the FODMAP protocol, which is often seen as the “go-to” dietary strategy for SIBO symptom management, however, it’s extremely restrictive and challenging to undertake, which is why it’s important to rule SIBO out with a test. What’s important to understand about any elimination diet is that whilst they can be incredibly helpful, they are designed to be temporary, which is why addressing possible dysbiosis and stress-related triggers should be an essential part of your approach.
3. Implement a gut-centred supplement regime
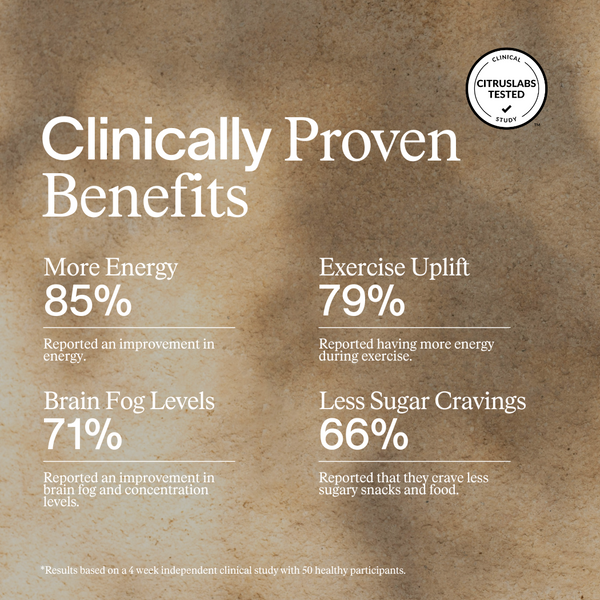
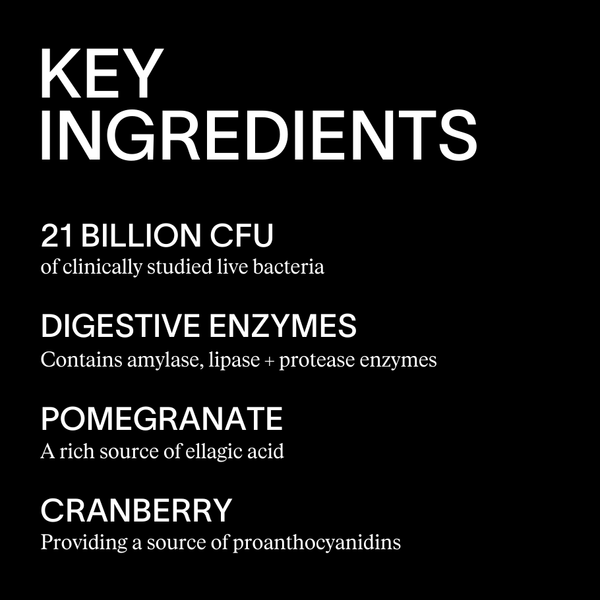
Research has shown that probiotics could hold the key when it comes to managing IBS. Enhanced Probiotic contains clinically studied strains that support IBS specifically, like Lactobacillus Lactis, Rhamnosus, and Plantarum, as well as Bifidobacterium Longum and Breve. In addition to combating IBS-related symptoms like bloating and pain, probiotics have also been shown to enhance gut motility, strengthen the intestinal lining, and reduce immune activation and inflammation.
An immune supplement like Cellular Defence can also prove useful in IBS, especially if it’s triggered or worsened by illness, infection and inflammation. It provides essential support to both your innate and adaptive immunity, thereby reducing any possible IBS-associated inflammation, and because antibiotic use can be so damaging to the gut, strengthening the immune system over time is important if you’re prone to getting ill.
4. Nurture the gut-brain axis
IBS symptom management is not just about food-based triggers, it’s also important to look at possible lifestyle factors, such as excessive stress. Stress management techniques have been associated with positive outcomes when it comes to IBS – so incorporating regular relaxation techniques such as deep breathing, meditation, mindfulness and yoga can help pull your strategy together.
Mindfullness isn’t just about stress management, it’s also key to notice how you’re eating your food – are you eating on the go, rushing your meals, eating with distractions, or barely chewing? All of these things will have an impact. Take the time to slow down, eat mindfully and chew food thoroughly to help to reduce bloating, gas, and digestive discomfort.
This article is for educational purposes only and the implementation of the theories and practices discussed is at the sole discretion of the individual. All advice given is not a substitute for medical advice, diagnosis, or treatment. If you have any concerns about your health, you should speak with your physician.